Our History
The New Zealand Resident Doctors' Association (NZRDA) was founded in 1985 to represent and advocate for resident doctors in New Zealand. Read on to learn more about our history and the impact we've had on improving conditions for doctors and healthcare in New Zealand.

-
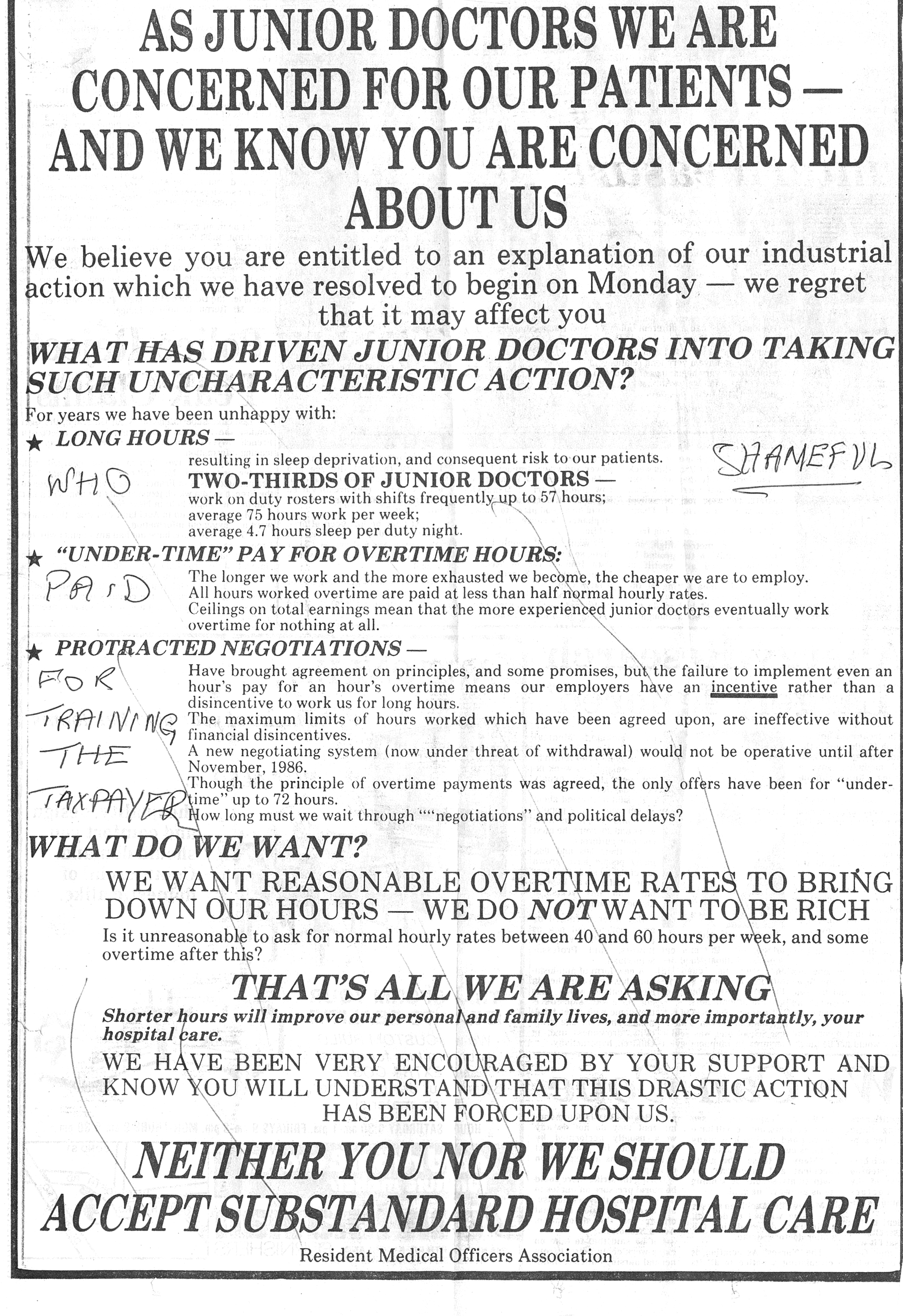
1985
Founded in 1985
- The New Zealand Resident Medical Officers Association (predecessor to the NZRDA) secures permission to represent RMOs.
- From there, it wins gains in working conditions, including a 12-hour shift limit, a 60-hour workweek cap, and guaranteed every-second weekend off.
-
-
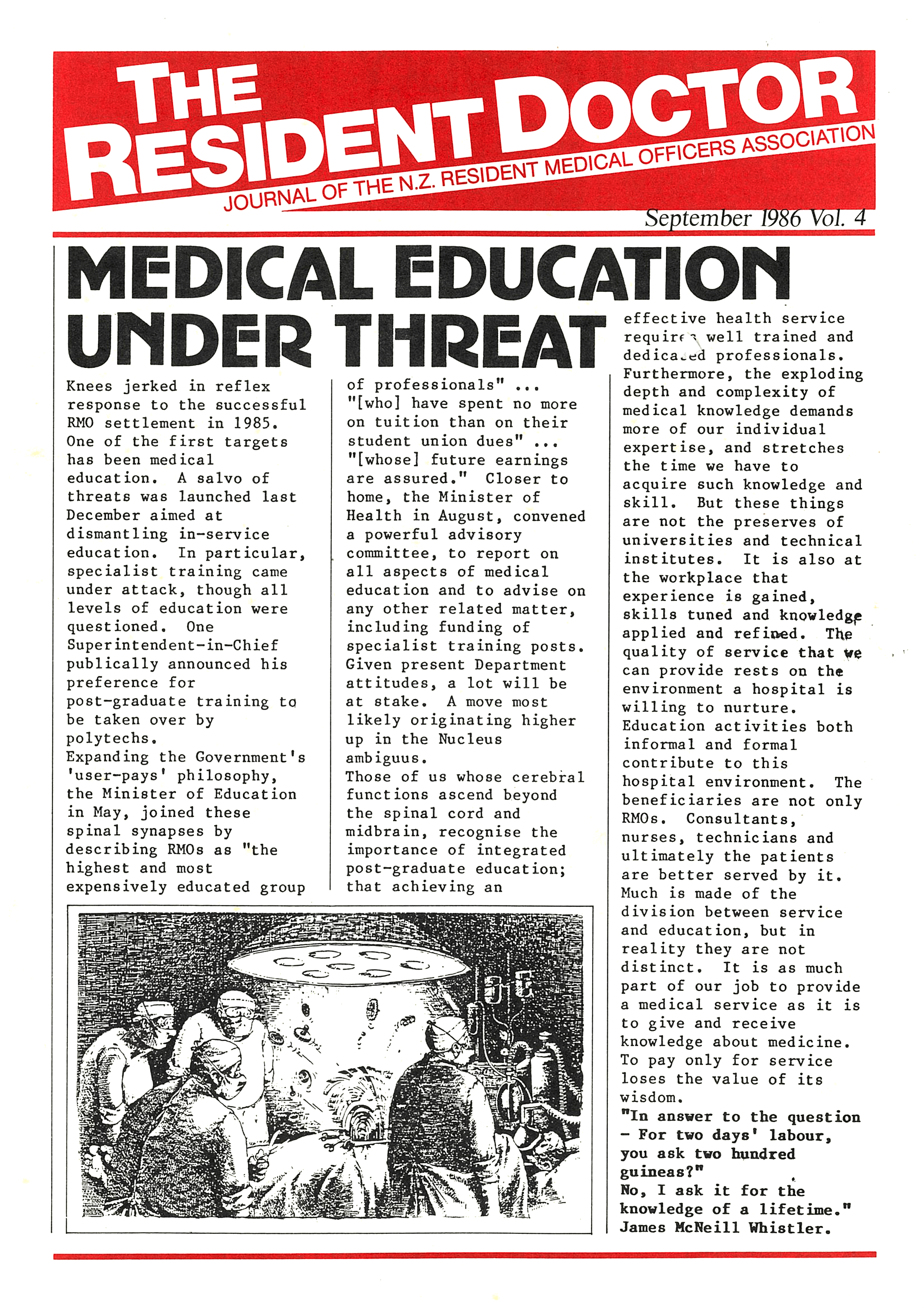
1986
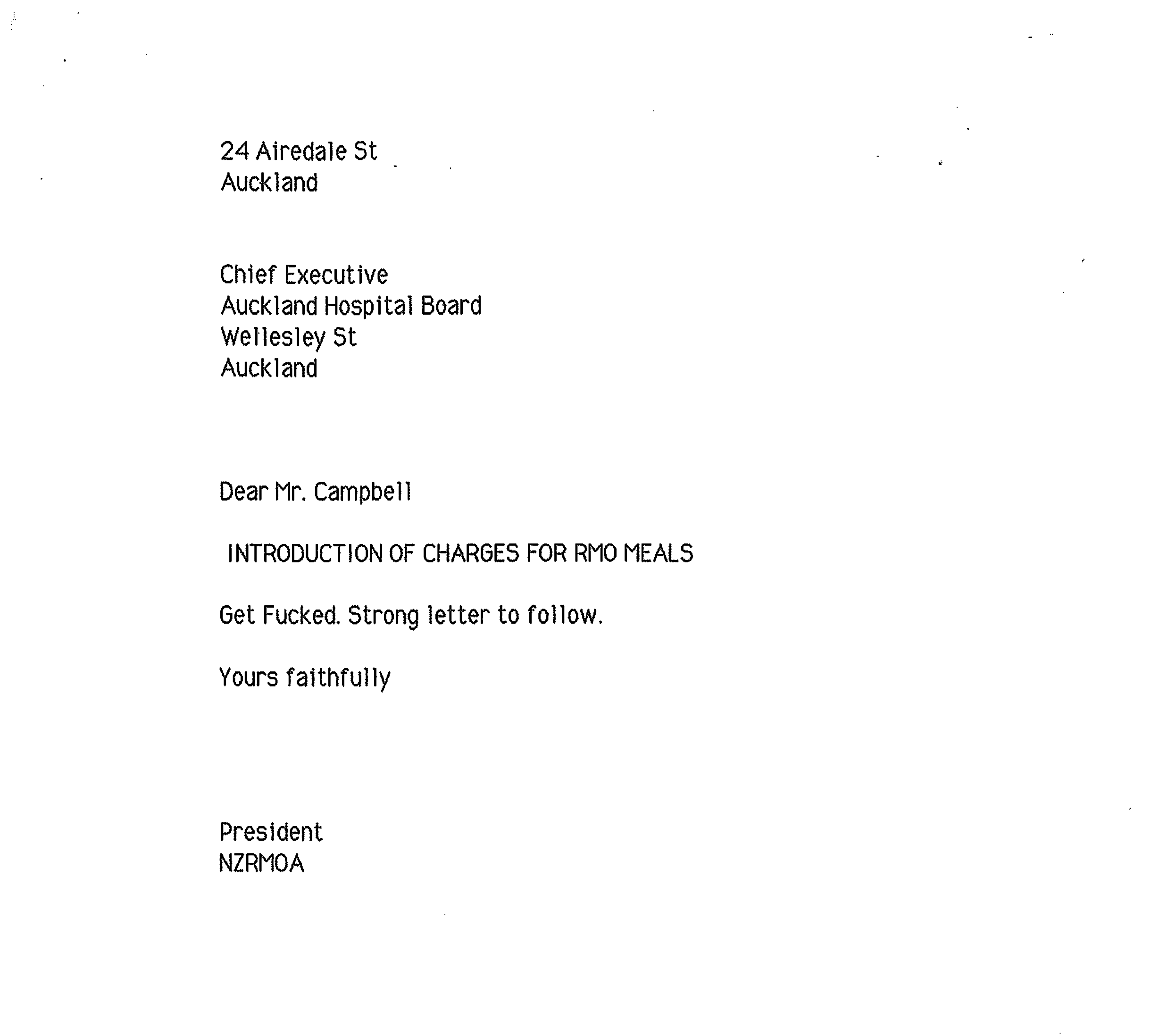
DBHS CUT ACCESS TO PAID MEALS
- Hospital Boards push to increase working hours to 16-hour shifts and a 72-hours a week. The NZRMOA agrees, but only with a commitment to reducing hours back to a 60-hour cap over time.
- RMOs face new challenges, with most DHBs—except Waikato—cutting access to paid meals on duty, prompting a legal battle in Auckland.
- Membership fees are set at just $5 per year.
-
-
1987
compensatory payments introduced
- Waikato DHB follows others in cutting paid meals, leading to the Waikato meals case in the Labour Court.
- NZRMOA secures a major win with the introduction of compensatory payments – ensuring RMOs are financially compensated for working beyond agreed hour limits.
-
1988
NZRDA launched the nationwide Meals Case
- NZRMOA launched the nationwide Meals Case, challenging the removal of paid meals for RMOs across the country.
-
1989
overtime and penal rates introduced
- NZRMOA secures a shift from compulsory payments to an industrial model, introducing overtime and penal rates. This change ensures RMOs are fairly compensated for the demands of their work.
-
1990
First salary model trialed in Auckland
- RMOs saw full reimbursement for APC (Annual Practising Certificate) and on-call telephone costs.
- NZRDA blocked universities from charging registrars fees, and successfully opposed proposals to withhold pay for protected teaching time.
- The Auckland Meals Case reached the High Court.
- Trainee Interns challenged the unfair practice of paying full-time university fees while working part-time.
-
1991
NZRDA won its first case UNDER THE ECA
- The Employment Contracts Act (ECA) was introduced, limiting union involvement and requiring single-employer bargaining.
- NZRDA won its first case under the ECA (Donnolly v. Otago Hospital Board), proving that employers couldn’t unilaterally change individual employment agreements.
- MATCH (the old ACE) ceased operations.
- NZRDA called for RMOs to be represented on the Medical Council of New Zealand (MCNZ).
- Strikes were carried out in multiple DHBs, with Bay of Plenty staging a four hour strike and Auckland, Christchurch, and Otago striking for nine days to settle their collective agreements.
-
1992
SOUTHLAND STRIKES
- Southland RMOs went on strike for six weeks, protesting the imposition of individual employment agreements and the refusal of the employer to negotiate a collective agreement.
- Training was officially recognised as a condition of employment.
-
$1,000 penalty introduced for any rostered shifts over 72 hours
-
cheaper alternative for indemnity insurance introduced
- The NZRDA introduced an indemnity insurance policy, reducing premiums from the $760 MPS was charging, to $400 per year.
-
1993
first Auckland Meals Case settled
- The first Auckland Meals Case was settled, with $1 million awarded for the issues before the Court.
- To cut costs, RDA subscriptions shifted to direct credit payments, avoiding a 2.5% fee charged by employers for salary deductions.
- The Gibbs and Stewart reports were released.
- A review of clinical training funding also took place.
-
1994
NZRDA introduced group life cover for all members
-
1995
- Medical education leave (MEL) was increased from 5 days to 6 weeks for sitting exams, and 2 weeks for diplomas.
- The new Medical Practitioners Act (precursor to our Health Practitioners Competence Assurance Act (HPCAA)) allowed RMOs to vote an RMO onto the Council (Marc Adams).
- TIs stopped being employees, and became students with stipends.
- The Health and Disability Commissioner (HDC) came into force.
- The NZRDA won legal action for cost transfers during college rotations and college membership fee reimbursements.
- The MCNZ proposal to levy first-year house officers was opposed.
-
All meals reinstated for RMOs
-
1996
- The Clinical Training Agency (CTA) (created taking funds from DHBs, then used to “buy back” RMO training) selects one RMO to be our voice.
- NZRDA successfully opposed the extension of provisional registration to 2 years.
- RMO income protection insurance was introduced.
- The average student loan reached $100,000.
-
1997
- A modified Calman report circulated, suggesting that RMOs come under the control of University Deans.
- NZRDA lobbied the Royal Australasian College of Surgeons (RACS) and the Royal Australasian College of Physicians (RACP) for generalist scopes of practice.
-
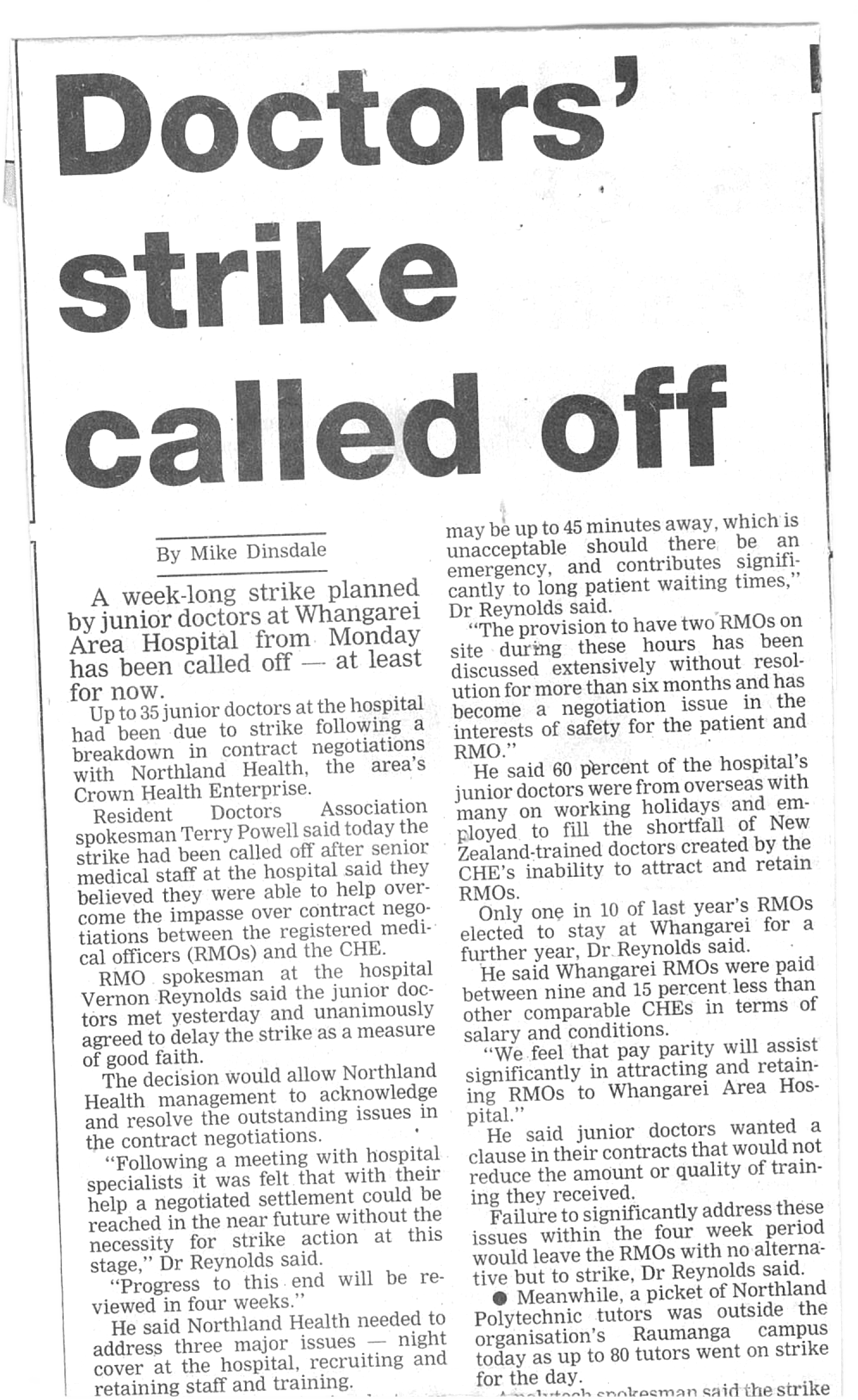
1998
NZRMOA became NZRDA
- 18 DHBs threatened strike action as Health and Hospital Service’s (HHS) attempted to exclude most RMOs from coverage by changing their job titles. Whanganui, Timaru, Nelson, and Tauranga had to strike to secure settlements.
- The first challenge was made against a college for unfair treatment of an RMO during training, followed by two further cases against employers for failing to support RMO training.
- Waikato finally paid for unrostered hours.
- Concerns were raised about the safety of 70-hour night shifts.
- Australia’s safer hours project was introduced, though it lacked legal enforceability.
- A new approach to avoid long days around weekends was implemented to meet the 60-hour weekly target.
-
1999
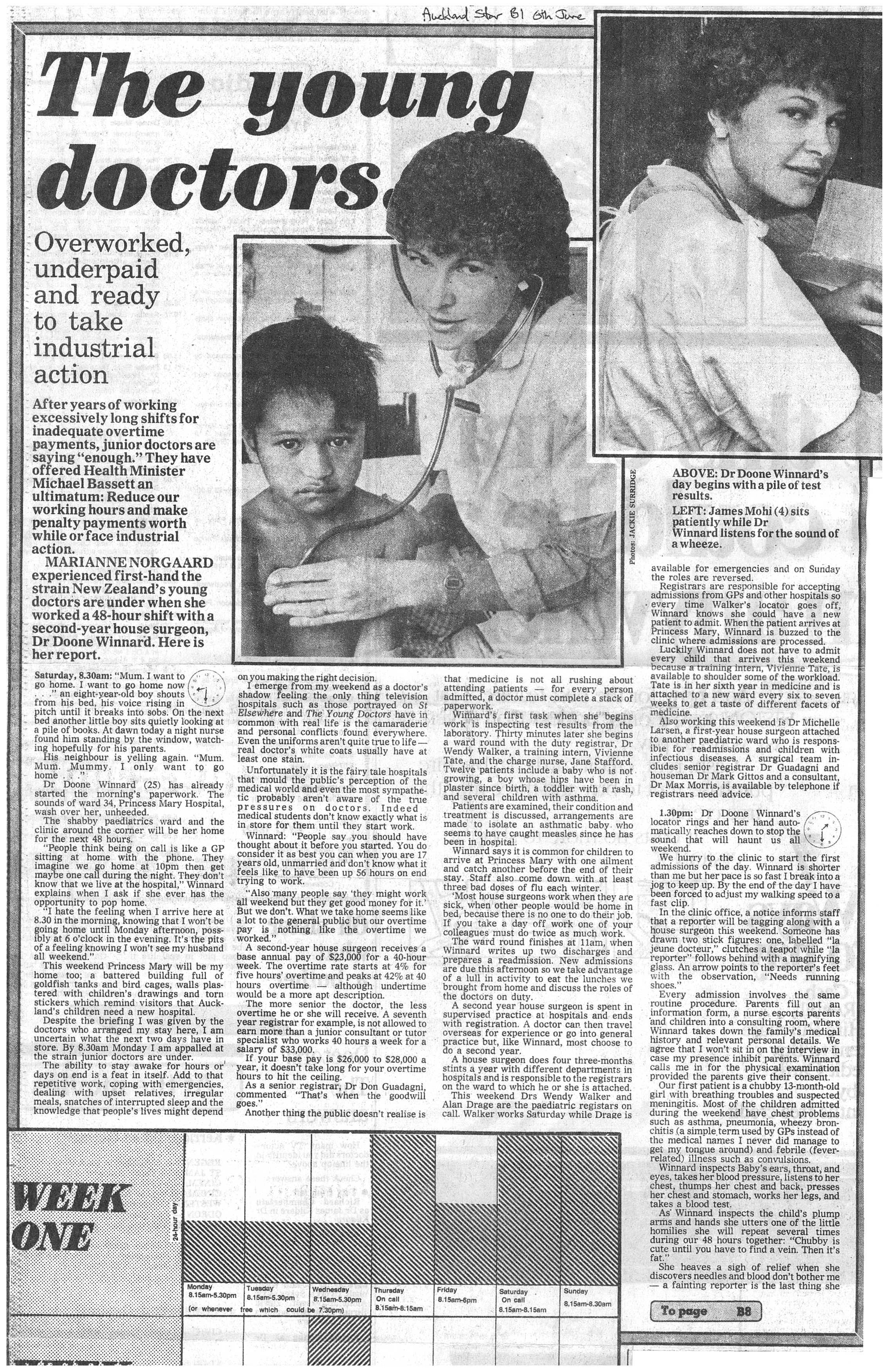
RMO recruitment and retention issues became critical
- RMO recruitment and retention issues became critical, with Middlemore Hospital first recognizing that too few RMOs led to excessive hours. This sparked concerns about cover for leave and working conditions. One manager stated, “…no other group of employees would accept working these conditions – my god imagine if we tried to get nurses to work like this, we would have a riot… and they get paid overtime!”
- Protected Training Time and reimbursement for training costs were introduced.
- The first joint working party, the Common Interest Working Group (CIWG), was established between HHSs and NZRDA, operating on consensus and commitment.
- Taranaki’s unilateral introduction of a draconian collective agreement for graduating TIs was met with an RMO strike in November.
- The Timms/Gollop Report in Waikato proposed replacing RMOs with Service Only Doctors (SODs).
- Wellington and Canterbury were identified as “bad employers” seeking to cut terms and conditions.
- The Northern Clinical Training Network (originally Northern Regional Alliance) formed a 3-employer collective agreement.
- The MCNZ Medical Education Committee began meeting RMOs directly for first-year accreditation reviews.
- The second Auckland meals case for compensation went back to court.
- NZRDA purchased 395 Dominion Road.
-
2000

Recruitment and retention issues worsened
- Recruitment and retention issues worsened, with the Auckland regional RMO workforce of 700 experiencing growing challenges.
- A joint investigation trip to Australia revealed a need for a 20% salary increase, but employers countered with only a 1.5% offer!
- Despite the Employment Contracts Act, NZRDA pursued national contract negotiations, leading to strikes in Northland, Palmerston, Whanganui, and Waikato, and ultimately, the G19 settlement. Auckland employers unsuccessfully tried to block the deal but settled for the same 20% increase under threat of strike action.
- The Employment Relations Act came into force in October 2000.
- Counties Manukau DHB employed 6 Service Only Doctors (SODs) at $120,000 each, working a 40-hour week.
- Rural health, pathology, and radiation oncology specialties were identified as areas of shortage.
- Post-settlement, HHSs and NZRDA agreed on a national process to address workforce planning and ensure consistent terms and conditions.
- The Medical Defense Union left the indemnity market.
- Auckland reinstated free meals for RMOs to limit liability in the 1999 court case. The National Meals payout liability was extended for another 4 years, with Wellington being the last HHS to finalize its schedule of entitled RMOs.
-

-
2001
no bargaining for the first time in NZRDA history
-
- NZRDA began investigating superannuation options for RMOs.
- Efforts to jointly progress issues from 2000 were hindered by Canterbury, Waikato, the 3 Auckland DHBs, and to a lesser extent, Taranaki and Southland. Canterbury continued to be the most difficult employer.
- The Wellington meals dispute was finalised, while Auckland appealed to the Court of Appeal after the Employment Court ruled in NZRDA’s favor.
- The Health Workforce Advisory Committee (HWAC) proposed lump sum payments to RMOs to help pay off student debt in exchange for years of service, but the government rejected it.
- NZRDA successfully took the “Dan the Uro Man” case, confirming that Australian registrars on rotation were entitled to training costs, highlighting the impact of ill-informed opinions from RMO Unit managers on DHB behavior.
- The locum pool was expanded.
-
2002
- NZRDA negotiated the first national multi-employer collective agreement for RMOs since the 1980s (excluding Gisborne where there were no RMOs were members).
- Changes to run descriptions were agreed upon only with the consent of all affected RMOs.
- A case involving a midwife, SHO, and O&G registrar found the registrar liable for decisions made.
- The Health Workforce Advisory Committee (HWAC) proposed relying on less qualified staff to address workforce issues.
- The meals legal process was finalized, with payouts underway, and unclaimed money was partially transferred to the Education Trust.
- NZRDA shifted to using personal email addresses for communication as DHBs blocked or read emails sent through their systems.
- DHBs sought to restrict training costs, introduce shifts at their discretion, and defined a long day as 10 hours.
-
2003
ACE introduced
- Hawke’s Bay was the last district to finally transition from the industrial model to a salary system.
- DHBs refused to provide changeover lists.
- There was a push to promote part-time training, and successful lobbying ensured that paid parental leave did not disadvantage RMOs during rotations.
- MCNZ affirmed that the person performing a procedure must obtain informed consent.
- Workplace violence, including bullying, was first exposed, and Auckland DHBs unsuccessfully attempted to introduce a cap on RMO meals.
-
2004
- The Doctors in Training Roundtable was established by the Minister without NZRDA representation.
- The Northland DHB 10/4 trial was underway, though interest from Otago, Hawke’s Bay, and Counties Manukau DHBs did not materialize.
- Southland’s crisis highlighted the key factors in RMO retention, while workplace bullying became a more visible issue.
- Legal action on 8.1.2, impacting anaesthetic registrars, was successful.
- Call-back payments were introduced at additional duty rates, separate from salary, along with an increase in on-call allowances.
- Rostering trials were agreed upon, limiting shifts to no more than 10 days and 5 nights, with 3 days off.
-
2005
Superannuation for RMOs included in the MECA
- Joint working group on workforce redesign was formed.
- The majority of meals money was transferred to the Education Trust.
- The UK concept of “Hospital at Night” emerged, alongside role substitution, primarily with nurses.
- DHBs raised the possibility of a “Greenfields MECA,” and the locum RMO whirlpool began to take shape.
- A national study by the Sleep Wake Research Centre examined RMO hours and fatigue, leading to the Safer Hours Conference.
- The Pan Professional Medical Forum was established.
- Northern Clinical Training Network (NCTN) became Auckland Regional RMO Services (ARRMOS).
-
2006
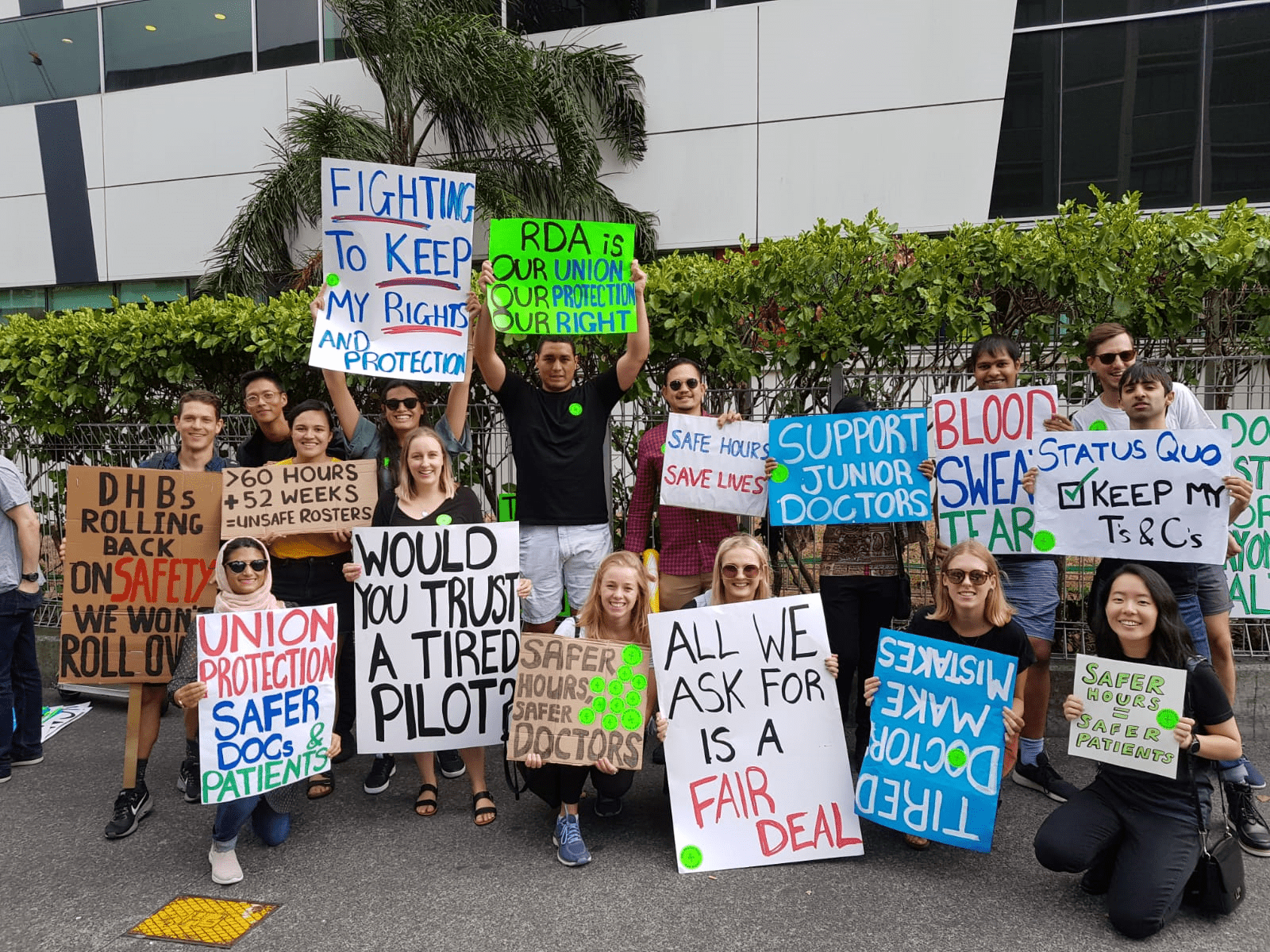
RMOs HELD their first-ever national strike
- Nigel Murray was appointed as Advocate to seek a Memorandum of Understanding (MoU) that would allow changes to the MECA, with employers holding the majority vote. Physical facilities were included in the MECA, along with an MoU to manage all trials of new work practices. Canterbury initiated “Hospital at Night” trials outside of the MoU.
-
2007
locum whirlpool reached its peak
- The locum whirlpool reached its peak, with $20 million spent in the Auckland region alone and 200 vacancies out of 900 positions.
- SMOs voted for strike action.
- RACS published “Standards for Safe Working Hours”.
- The MoU explored clinical handovers, IV-line insertion by non-RMOs, safer hours including 10:4 rostering, access to ED experience, and Career Pathway Planning. However, Taranaki DHB ignored the MoU when changing work practices.
- The Medical Training Board (MTB) was formed.
- DHBs confirmed their commitment to part-time training opportunities in the MECA.
-
2008
Strike action required to settle the MECA
- The RMO Commission was formed, proposing a single-employer model as an option, but it was ultimately not adopted. Auckland DHBs investigated the single-employer concept.
- Strike action was required to settle the MECA, despite opposition from the Council of Trade Unions President.
- An agreement on locum rates was made, capping them at $150.00 per hour.
- The RNZCGPs ceased offering seminar-only options for GP registrars, with college registrars on a stipend lower than the MECA rate and not considered employees.
- NZRDA reaffirmed its commitment to the name “Resident Doctors” or RMOs, explicitly avoiding “junior doctors”.
-
2009
anti-bullying campaign LAUNCHED
- Canterbury moved to unilaterally restrict meal entitlements, but legal action resulted in a victory for NZRDA.
- The new Medical Practitioners Act introduced General and Vocational registration.
- NZRDA launched an anti-bullying campaign and secured coverage for Public Health registrars at the Ministry of Health.
-
2010
TRANSITIONED to interest-based bargaining
- The union moved to interest-based bargaining, rejecting a 2% pay rise in favor of using the funds to hire more RMOs, but this proposal was rejected by employers.
- The cross cover outside of ordinary hours (XCOOH) breach issue first emerged.
- The Auckland regional RMO unit faced issues with non-compliance, poor rostering, and communication. Auckland DHBs attempted to force RMOs to accept individual employment agreements.
- Employers no longer supported the 2007 MoU, and they unsuccessfully tried to block NZRDA’s initiation of bargaining for 4 MECAs. Employers tabled a Greenfields MECA, leading to NZRDA’s first publicity campaign with TV ads and the interactive website “Treating Doctors Well, Treating People Well.”
- A voluntary bonding scheme was introduced.
-
RDA celebrated its 25-year anniversary
-
2011
The first GPEP1 Registrars joined the program
- The issue of limiting to a maximum of 4 nights with 3 sleep recovery days was formally raised.
- A decision was made to employ GPEP registrars (effective Dec 2012) by DHBs, but this was later changed to RNZCGP. A trial of Physician Assistants at Middlemore Hospital failed.
- Health Workforce NZ, established in 2010, became more active.
- The indicative training career planning process was first introduced.
-
2012
NZRDA negotiated the first GPEP CA
- RNZCGP became the employer of GPEP registrars, offering inferior individual employment agreements (IEAs) compared to DHB-employed registrars, and NZRDA negotiated the first GPEP CA, covering 174 GPEP1 registrar positions.
- Best Practice Advocacy Centre New Zealand (BPAC) recertification was introduced by MCNZ for House Officers.
- The voluntary bonding scheme paid its first group of 24 enrolled RMOs.
- Additional Continuing Medical Education (CME) provisions for senior registrars were added to the MECA.
-
2013
- The MECA app was introduced for members, providing a guide to the MECA.
- The Auckland region initially cut first-year positions from 152 to 50, but after pressure, they increased it to 120, while the rest of New Zealand added 32 more.
- MCNZ failed to extend provisional first-year registration to two years.
-
2014
Strike action narrowly averted
- The third round of interest-based bargaining for the MECA saw a potential settlement overturned by employers, who sought the ability to unilaterally change run descriptions and salaries. Strike action was narrowly averted with a one-year suspension of changes to run descriptions.
- NREG (National Resident Doctor Engagement Group) collapsed amid bargaining tensions.
- In 2014, there were 3,200 RMOs employed in DHBs nationally.
- MCNZ introduced a “requirement” for House Officers to undertake a Community-Based Attachment (CBA).
- Electronic balloting was introduced.
- Six DHBs converted House officer rosters to 4 nights with 3 sleep days off.
- Safety guidelines for smart device use in the workplace were circulated.
- MCNZ’s Eport for GPEP 1 & 2 was introduced.
- Dunedin and Auckland lost Intensive Care Unit (ICU) accreditation to train specialists.
-
2015
Not our responsibility to help
- Pipeline work secured enough first-year placements to accommodate the increased medical school output.
- Accreditation was at risk for first-year training in Otago, Obstetrics & Gynecology in Waikato, and Orthopedics in Otago.
- The RDA also launched a training survey to gather further insights.
-
2016
safer hours campaign progress
- NZRDA’s safer hours campaign achieved a maximum of 10 days with 4 nights of sleep and 3 recovery days on acute rosters.
- Around 20% of house officers undertook a Community-Based Attachment (CBA), but Auckland and Waitemata actively resisted offering this opportunity.
- The RDA also conducted a joint review of the Cognitive Institute’s anti-bullying program in Melbourne.
- Social media was actively used for the first time in a NZRDA campaign.
- A template IEA was provided for public health registrars working outside DHBs.
- MCNZ rejected the RDA’s request for representational positions on their medical education committee, maintaining that 3 RMOs out of 15 members was sufficient.
- The RDA lobbied to remove confidential references and referees to reduce the fear of career retribution.
-
2017
MCNZ's 10-week rule rejected
- NZRDA first objected to the MCNZ’s 10-week rule, which required first-years to work 10 out of 13 weeks on any run to gain general registration. Waikato failed accreditation for first-years with MCNZ.
- The NZRDA launched free access to Headspace, a wellbeing app, for members.
- DHBs accepted the abolition of confidential references or referees, set to commence in 2018.
- The training survey, first launched in 2015, was repeated.
- A review of relief positions led to an increase in reliever roles.
-
2018
DHBs attacked the 2/3 agreement provision
- During bargaining, DHBs attacked the 2/3 agreement provision, with STONZ agreeing to a 1/3 disagreement provision (this was their first CA), leading to industrial action.
- NZRDA raised “Teach the Teachers” courses as options for RMOs and repeated the Bullying and Sexual Harassment survey.
- The NZRDA successfully improved the Eport for HOs, with the 10-week rule becoming a “guideline.”
- The Transition from Trainee Intern to House Officer program was introduced, including the House Officer Teaching TIs (HOTTI) program for new HOs run by delegates.
-
2019
Capital & Coast tried to reduce meal options
- Capital & Coast DHB tried to reduce meal options to predetermined “combo” options, but this was unsuccessful.
- NZRDA conducted research comparing time-based training systems versus competency-based training.
- A clinical governance conference was held by the NZRDA, followed by “runs” for RMOs.
- RDA researched the barriers to part-time employment for RMOs.
- During bargaining, the focus for the third consecutive round was on remuneration, decreasing schedule 10, and removing the BP agreement provision. This led to further strike actions, with TV ads being featured in the dispute. Two-day strikes in January and February resulted in facilitation, and the MECA was ratified in August.
- A Section 62 dispute occurred over CA coverage for new employees.
- A legal case affirmed RMOs’ rights to parental leave payments during rotations.
-
2020
- The Ministry of Health introduced healthy eating guidelines and attempted to influence meals provision.
- Canterbury DHB unsuccessfully tried to reduce access to meals.
- The COVID-19 pandemic had a significant impact.
- The formation of Health New Zealand (HNZ) was also announced.
- There was consultation over changing the RMO year, but it was largely seen as window dressing.
- The research comparing competency-based versus time-based training was completed, with further engagement with MCNZ to remove the 10-week rule.
- Part-time employment guidelines were agreed with DHBs.
- All House Officers (HOs) were expected to have CBAs by 2020, Auckland/Waitemata was still behind on creating runs to comply.
-
2021
- The MECA was settled, including:
- Provisions for scrubs
- Improved weekend-off provisions for ED and ICU
- Time off for RMO’s on-call over weekends
- Cessation of salary deductions for RDOs
- ED roster reviews were conducted, leading to an increase in RMO full-time equivalent (FTE) in many departments.
- Cross cover outside of ordinary hours (XCOOH) became a significant issue.
- NZRDA surveyed first-year RMOs to assess whether DHBs met MCNZ accreditation requirements.
- The RMO year dates were changed after previous years consultation.
- The MECA was settled, including:
-
2022
NZRDA challenged the RACP
- NZRDA challenged the RACP oral pediatrician exam for deficiencies, including racial bias, and also challenged MCNZ accreditation processes.
- Bargaining with Te Whatu Ora took place amid the cost-of-living crisis, with the focus on:
-
-
Gaining support to increase medical school placements.
-
Supporting the transition from RMO to SMO with continuous employment.
-
Securing pay for TIs.
-
Working towards a 1:3 weekend for ICU/ED, a max of 25% nights, and a minimum B salary.
-
- The ED roster review continued, increasing ED Full-Time Equivalent (FTE)
- Reusable water bottle project was trialed.
- Health New Zealand (HNZ) established.
- NZRDA student chapter was created.